Most men will likely agree that prostate health is an important yet often overlooked aspect of wellness.
Advancements in robotic surgery are transforming treatment options for common prostate conditions like enlargement and cancer, offering less invasive procedures with better outcomes.
This article explores the evolution of urology and robotic prostate surgery, comparing traditional and robotic approaches while identifying criteria for choosing an experienced surgeon to treat prostate disease.
Introduction to Robotic Surgery for Prostate Conditions
Robotic surgery, specifically the da Vinci surgical system, has transformed the landscape of urologic care. This advanced technology offers unmatched precision, control, and access compared to traditional open and laparoscopic techniques. For conditions like prostate cancer, benign prostatic hyperplasia (BPH), and prostatic enlargement, a robotic approach provides numerous advantages.
Evolution of Urology and Prostate Robotic Surgery
The integration of robotics into urologic care has rapidly accelerated over the past two decades:
- In 2000, the FDA approved the da Vinci system for general laparoscopic surgery. This opened the door for urologists to leverage the technology.
- By 2008, over 50% of radical prostatectomies were performed robotically. Robotic prostate surgery had become mainstream.
- Today, the da Vinci robotic system is used in 85-90% of prostate cancer cases requiring surgery. It has become the standard of care.
This exponential growth underscores the value robotic surgery brings to effectively treating prostate conditions.
Comparing Traditional and Robotic Prostate Cancer Treatment
For prostate cancer, robotic surgery offers distinct benefits over open radical prostatectomy:
- Less blood loss: Average blood loss is reduced from over 1 liter to just 75mL. This significantly lowers transfusion rates.
- Shorter hospital stay: Patients typically leave the hospital in 1 day rather than 2-3 days.
- Quicker recovery: Most men regain urinary control in 4-6 weeks rather than 8-12 weeks.
- Lower risk of ED: Erectile dysfunction rates are 25-30% lower compared to open surgery long-term.
Ultimately, a robotic prostatectomy facilitates better outcomes all around.
Identifying the Best Urologist for Prostate Cancer and BPH
When selecting a urologic surgeon for prostate issues, key factors to evaluate include:
- Board Certification: Confirm the doctor is board-certified in urology. This ensures extensive specialized training.
- Clinical Focus: Seek out a urologist who concentrates on prostate conditions and robotic surgery. Their experience level is vital.
- Hospital Privileges: A top doctor should have privileges at premium local hospitals and outpatient surgical centers.
- Patient Reviews: Read reviews and testimonials to understand real-world results and patient satisfaction.
- Bedside Manner: Schedule a consultation to determine if the urologist's communication style aligns with preferences.
Prioritizing these elements helps identify the most qualified prostate specialist for individual needs.
The Impact of Robotic Surgery on Prostate Enlargement Treatment
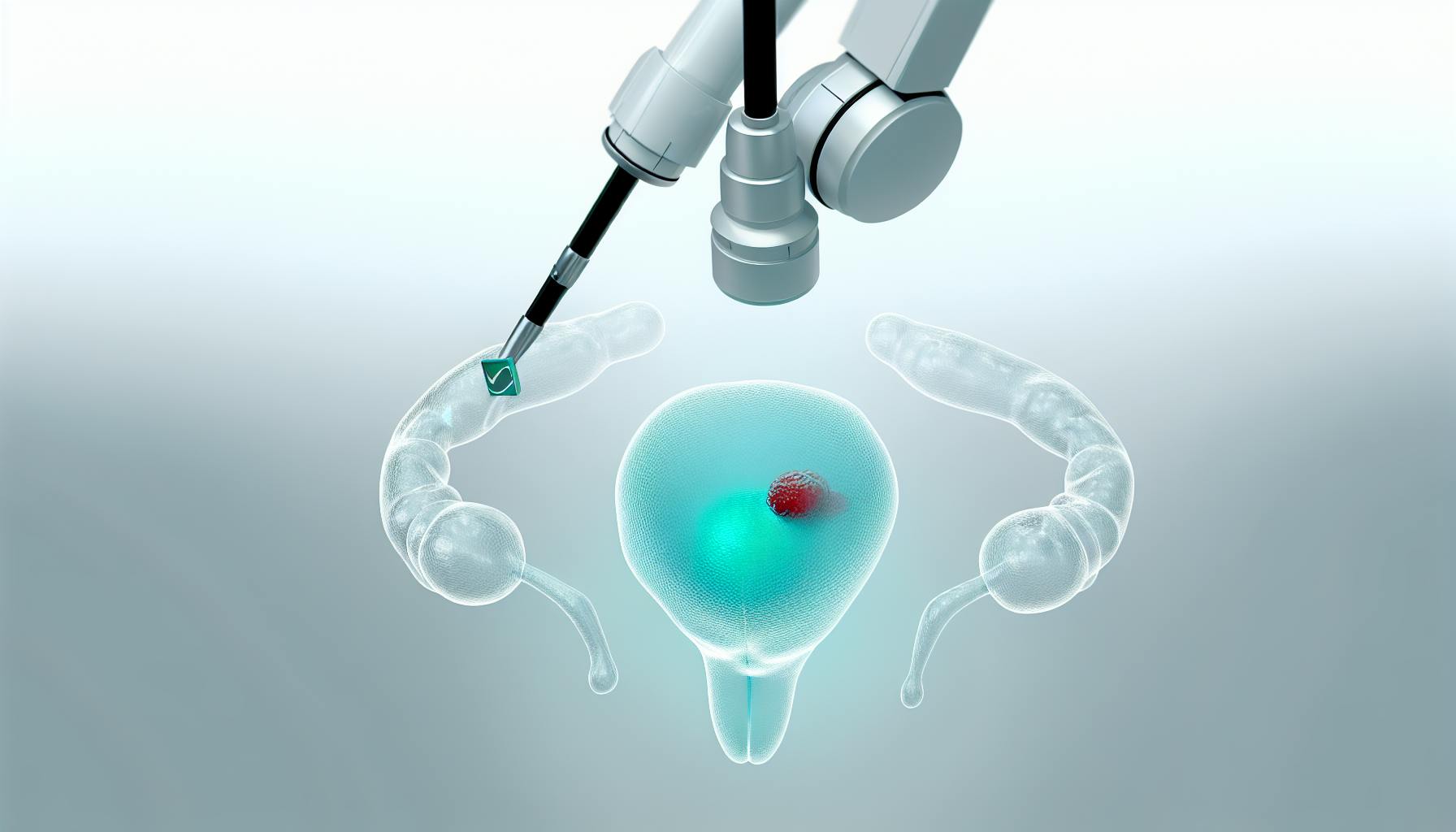
For benign prostate enlargement and associated lower urinary tract symptoms (LUTS), robotic simple prostatectomy is transforming treatment. This technique for removing obstructing prostate tissue provides advantages over traditional transurethral resection of the prostate (TURP), including:
- Reduced bleeding: Average blood loss is less than 25mL compared to over 500mL for TURP.
- Lower complication rates: Instances of erectile dysfunction, urinary incontinence, and stricture are minimized.
- Shorter catheter times: Post-op catheterization averages just 5 days rather than 2-3 weeks.
- Quicker recovery: Most patients return to normal activity in 2 weeks instead of 4-6 weeks.
Robotic surgery is quickly being recognized as a superior technique for addressing benign prostate enlargement.
What does a urologist do for prostate?
A urologist is a physician who specializes in diagnosing and treating conditions related to the urinary tract system and male reproductive organs like the prostate. Here are some of the key things a urologist does regarding prostate health:
- Diagnosing prostate conditions - A urologist can help diagnose various prostate issues like enlarged prostate (BPH), prostatitis, and prostate cancer. They utilize tests like digital rectal exams, PSA tests, biopsies, imaging scans, etc. to determine the cause of prostate symptoms.
- Treating benign prostate diseases - For benign diseases like BPH, a urologist may prescribe medications or recommend minimally invasive procedures like transurethral microwave thermotherapy or transurethral needle ablation. For severe BPH, they perform surgical procedures like transurethral resection of the prostate (TURP) or photoselective vaporization of the prostate (PVP).
- Treating prostate cancer - If prostate cancer is detected, the urologist will determine the stage and grade to map out the best treatment plan. This may involve active surveillance, radiation therapy, robotic radical prostatectomy surgery, etc. They have specialized expertise in surgical and non-surgical cancer treatments.
- Managing side effects - A urologist helps patients deal with side effects of prostate treatments like erectile dysfunction or incontinence using medications, devices, physical therapy, etc.
- Ongoing monitoring - They will monitor PSA levels and disease progression over time to ensure the prostate treatment is working effectively or detect any recurrence needing further management.
In summary, urologists have comprehensive training in prostatic conditions, utilizing various diagnostic tests and advanced treatment modalities tailored to each patient's unique health profile and needs regarding benign prostate diseases or prostate cancer. Their specialized knowledge helps provide optimal prostate care.
What are the 5 warning signs of enlarged prostate?
An enlarged prostate, also known as benign prostatic hyperplasia (BPH), can cause several bothersome urinary symptoms. Here are 5 of the most common warning signs that may indicate an enlarged prostate:
-
Dribbling at the end of urinating
The inability to fully empty the bladder can cause urine to continue to dribble out after you think you have finished urinating. This symptom is known as post-void dribbling.
-
Inability to urinate (urinary retention)
An enlarged prostate can block the flow of urine out of the bladder, making it difficult or even impossible to urinate. This is called acute urinary retention and is considered a medical emergency.
-
Incomplete emptying of your bladder
Related to urinary retention, many men with BPH find they can never fully empty their bladder even if they can urinate. Over time, residual urine left in the bladder can increase the risk of infection.
-
Frequent urination at night (nocturia)
Waking up frequently during the night to urinate, sometimes 2 or more times per night, can indicate BPH. This happens because the bladder becomes overly sensitive as it tries to compensate for incomplete emptying.
-
Pain with urination or bloody urine
While less common, some men with an enlarged prostate experience painful urination, decreased urine stream, and bloody urine. This may indicate an infection or other prostate condition.
If you experience any of these urinary symptoms, schedule an appointment with a urologist. Catching and treating an enlarged prostate early can help prevent complications. A urologist has specialized training to accurately diagnose the cause and create an effective treatment plan.
What are the first signs of a prostate problem?
See your doctor right away if you experience any of the following symptoms, which may indicate a prostate issue:
- Frequent urge to urinate
- Getting up many times during the night to urinate
- Blood in urine or semen
- Pain or burning during urination
- Painful ejaculation
- Frequent pain or stiffness in lower back, hips, pelvic/rectal area, or upper thighs
- Dribbling of urine
These symptoms should not be ignored, as they can signify conditions like benign prostatic hyperplasia (BPH) or prostate cancer. It's important to meet with your doctor, who can perform tests like a digital rectal exam and PSA blood test to determine if your prostate is enlarged or if there are any abnormalities.
Based on your test results and evaluation, your doctor may recommend treatment options such as prescription medications, minimally invasive surgeries, or more aggressive surgical procedures. Catching prostate issues early is key - you greatly improve outcomes by seeking medical advice promptly when these urinary and other troubling symptoms arise. Don't delay, as waiting can allow the condition to progress.
What is the best thing to drink for your prostate?
Staying properly hydrated is important for overall health, including prostate health. Here are some of the best drinks for the prostate:
- Water - Staying hydrated is crucial. Aim for at least eight 8-ounce glasses of water per day. Dehydration can worsen urinary symptoms.
- Green tea - Contains antioxidants that may help reduce inflammation. Studies show green tea may benefit prostate health.
- Pomegranate juice - Rich in antioxidants. Some research indicates it may slow prostate cancer growth.
- Cranberry juice - Helps prevent urinary tract infections, which can lead to prostatitis. Choose low-sugar versions.
- Tomato juice - Good source of lycopene, an antioxidant that may play a role in prostate health. Low sodium is preferred.
Avoid or limit alcohol and caffeinated beverages like coffee or soda, as these can irritate the prostate. When symptomatic, reducing fluid intake in the evening may help minimize nighttime urinary frequency.
Staying hydrated with water and nutrient-rich beverages supports overall health. Discuss options with your urologist to determine what's best for your prostate.
sbb-itb-89ec482
Understanding Prostate Conditions
This section provides an overview of common prostate conditions like benign prostatic hyperplasia (BPH) and prostate cancer, including symptoms, diagnosis, and treatment options.
Symptoms and Causes of Prostate Conditions
The most common symptoms of prostate conditions include:
- Frequent urination, especially at night
- Difficulty starting or stopping urination
- Weak urine stream or flow
- Straining to urinate
- Blood in urine or semen
These symptoms are often caused by benign prostatic hyperplasia (BPH), which is an enlargement of the prostate that puts pressure on the urethra. BPH is common in older men. The exact causes are unknown but may involve hormone changes or abnormal cell growth.
Other prostate conditions like prostatitis (inflammation of the prostate) and prostate cancer can cause similar urinary symptoms. That's why it's important to see a urologist for an accurate diagnosis.
Diagnosis of Prostate Conditions: From PSA to Biopsy
Diagnosing prostate conditions usually starts with a digital rectal exam and PSA (prostate-specific antigen) blood test. The PSA test measures levels of a protein made by the prostate. High or rising levels may indicate an enlarged prostate or prostate cancer.
If these screening tests raise concerns, the urologist may recommend further tests like:
- Urine and semen tests to check for infection or blood
- Imaging tests like transrectal ultrasound to examine the prostate
- Urodynamic tests to assess bladder function
- Cystoscopy to view the urethra and bladder using a tiny camera
- Prostate biopsy to extract small tissue samples for examination under a microscope
These medical tests help determine if symptoms are due to BPH, prostate cancer, infection, or other conditions.
Navigating Prostate Cancer Treatment Near Me
If diagnosed with prostate cancer, it's important to find experienced specialists nearby. Key factors in choosing prostate cancer treatment include:
- Board certification: Confirm the doctor is board-certified in urology with a fellowship in oncology. This expertise ensures you get the most advanced care.
- Hospital affiliations: Academic medical centers and NCI-designated cancer hospitals have the latest technology and clinical trials unavailable elsewhere.
- Surgical case volume: Seek out high-volume prostate surgeons performing at least 50+ cancer operations per year. Their extensive experience leads to better outcomes.
- Multidisciplinary care: Get opinions from various experts like urologists, radiation oncologists, and medical oncologists to customize treatment.
- Support services: Look for robust counseling, nutrition, and follow-up care to manage side effects and recovery.
Doing research upfront helps find the most qualified prostate cancer treatment near you.
Benign Prostatic Hyperplasia Treatments and Innovations
For early-stage BPH, doctors often prescribe alpha-blockers or 5-alpha-reductase inhibitors to relax muscles around the prostate and improve urine flow.
As the prostate grows larger, minimally invasive surgical options include:
- Transurethral microwave thermotherapy to destroy excess prostate tissue using heat
- Transurethral needle ablation which injects low-level radiofrequency energy into the prostate
- UroLift to pin back enlarged prostate tissue pressing on the urethra
For severe BPH, traditional surgery called transurethral resection of the prostate (TURP) removes prostate tissue piece by piece through the urethra. This can cause side effects like retrograde ejaculation.
A newer option is robotic simple prostatectomy which removes the entire enlarged prostate in one piece through small abdominal incisions. This maintains sexual function while opening up the urethra for improved urination.
Robotic techniques provide a highly magnified 3D view inside the body, precision movements scaled to the surgeon's hand motions, and tiny incisions for faster recovery. These technological advances make robotic simple prostatectomy a state-of-the-art solution for treating benign prostatic hyperplasia.
The Robotic Approach to Prostate Surgery
This section examines the use of robotic surgery for treating prostate conditions. We'll explore the benefits, find expert surgeons, analyze costs, and discuss emerging techniques.
Advantages of Robotic Prostatectomy for Cancer Treatment
Robotic prostatectomy offers several advantages over open surgery:
- Enhanced visualization with 3D, 10x magnification allowing precise dissection
- Greater range of motion with robotic arms allowing access to confined spaces
- Smaller incisions leading to less pain, bleeding, and faster recovery
- Shorter hospital stay (1-2 days vs 2-4 days with open surgery)
- Lower risk of impotence (17-20% vs 30-60% with open surgery) and incontinence (4-8% vs 6-20%)
These benefits often lead to better cancer control and quality of life outcomes. Studies show similar or lower positive margin rates versus open and laparoscopic techniques.
Finding Robotic Prostate Surgeons Near Me
When researching surgeons, look for these credentials:
- Board-certified urologist with fellowship training in robotic surgery
- Experience performing >100 robotic prostatectomies
- Regional/national recognition and awards in the field
- Hospital with high-volume robotic surgery program
Also check patient reviews and ask about communication style. An expert surgeon should explain options clearly and customize the approach based on your priorities.
Cost-Effectiveness: Average Cost of Robotic Prostatectomy
The average cost of robotic prostatectomy ranges from $15,000-$25,000 in the U.S. This is more expensive than open surgery ($10,000-$15,000) but has a lower risk of complications and quicker recovery.
Over a lifetime though, the long-term side effects avoided with a robotic approach can lead to cost savings from better health outcomes. Check insurance coverage and speak to financial coordinators when budgeting for surgery.
Emerging Trends: New Surgery Techniques for Prostate Cancer
Exciting areas of research include:
- Focal therapy to target just the tumor while preserving erectile function
- Nanoknife technology using electricity to destroy cancer cells
- MRI-US fusion for enhanced imaging during surgery
- Single-port and Natural Orifice Transluminal Endoscopic Surgery (NOTES) further minimizing invasiveness
Patient participation in clinical trials allows early access to these latest robotic techniques.
Postoperative Care and Recovery
This section outlines the post-surgical journey, focusing on recovery and long-term care following robotic prostate surgery.
Managing Expectations: Life After Robotic Prostate Surgery
Patients can expect a 1-2 day hospital stay after robotic prostate surgery. Typical recovery time is around 2 weeks, though patients are encouraged to pace themselves and not rush back to normal activity. Potential short-term effects include pain/discomfort, catheter use, and incontinence. With time and pelvic floor rehabilitation, most patients see great improvement within 3-6 months. It's important to have realistic expectations about recovery to avoid frustration.
Monitoring for Recurrence: Prostate Cancer Follow-Up
After robotic prostatectomy, regular check-ups are crucial to monitor PSA levels and watch for potential cancer recurrence. Typically, PSA is measured quarterly for the first year, biannually for years 2-5, and annually thereafter. If PSA rises, additional tests and potential radiation may be required. Catching recurrence early leads to better outcomes.
Physical and Emotional Support During Recovery
Physical therapy helps retrain pelvic floor muscles impacted by surgery. Support groups connect patients with others going through similar experiences. Counseling provides an outlet for the fear/anxiety of facing cancer. Utilizing these resources ensures patients don't feel alone during recovery.
Long-Term Outcomes: Success Rates of Robotic Surgery for Prostate Conditions
Multiple studies show ~90% of patients are cancer-free 5 years post-op. 10-year recurrence rates are only ~10-15%. Patients report preserved sexual/urinary function. Robotic prostatectomy has revolutionized treatment, providing effective cancer control and lifestyle preservation for thousands of patients.
Seeking Care from an Experienced Robotic Surgeon
Robotic surgery has revolutionized treatment options for prostate conditions. When considering surgery, it is critical to select an experienced, specialized surgeon to perform the delicate procedure.
Criteria for Choosing the Best Prostate Surgeon
Several key factors to evaluate when selecting a prostate surgeon include:
- Surgical Volume: A high-volume surgeon who regularly performs prostate procedures will have greater proficiency and more consistent outcomes. Ask about the number of surgeries conducted annually.
- Robotic Surgery Expertise: Seek out a surgeon with extensive robotic surgery experience specifically for prostate cancer and BPH. Ask how long they have performed robotic procedures.
- Outcomes Data: Reputable surgeons should provide statistics on positive outcomes, cancer cure rates, and complication rates from past surgeries. This offers reassurance.
- Hospital Affiliations: Academic medical centers and highly-ranked hospitals have rigorous credentialing standards for affiliated surgeons. This signals advanced skill level.
- Patient Reviews: Read reviews from past patients on factors like bedside manner, communication style, and attentiveness. These provide insight into the care experience.
Questions to Ask Your Prostate Cancer Doctor
Essential questions to ask any prostate cancer specialist you consult include:
- What are all the treatment options for my cancer stage and grade? Do you recommend surgery, or are other options like radiation or active surveillance preferable?
- If surgery, do you advise an open or robotic procedure? Why?
- How many robotic prostatectomies do you conduct per year? What is your positive margin and recurrence rate?
- Which surgical approach would you use (perineal, retropubic, or single-site surgery)? Why is this approach optimal?
- How quickly after surgery can I expect to regain urinary control and sexual function?
The Role of a Urologist Prostate Expert in Robotic Surgery
As genitourinary specialists, experienced urologists offer unique expertise in treating prostate issues. For robotic surgery, a dedicated uro-oncology surgeon provides:
- Specialized knowledge of the genitourinary system's anatomy and related cancers
- Understanding of the latest innovations in robotic prostate surgery techniques
- Meticulous nerve-sparing surgical skills to preserve sexual function
- Holistic perspective spanning diagnosis, surgery, and post-operative care
- Emphasis on communication, patient education, and continuity of care
Locating the Best Prostate Surgeon Near Me
To find a reputable prostate surgeon in your area:
- Search urology department websites of highly ranked community and teaching hospitals
- Check "Top Doctor" listings in local publications and medical associations
- Look for prostate cancer specialty certifications from the American Board of Urology
- Use referral services from prostate cancer support groups and foundations
Identifying an expert robotic surgeon for your prostate operation is worth the effort - an experienced specialist can translate into better outcomes.
Conclusion: Embracing the Future of Prostate Treatment
Recap of Robotic Surgery Benefits in Urology
Robotic surgery has transformed the landscape of prostate treatment over the past two decades. Compared to open surgery, robotic procedures offer significant advantages:
- Enhanced visualization and precision due to 3D HD cameras and wristed instruments
- Less blood loss and reduced pain thanks to smaller incisions
- Shorter hospital stays and faster recovery times
- Lower risk of impotence or incontinence side effects
These benefits have made robotic surgery the gold standard for prostate cancer and BPH surgeries. Patients can undergo complex procedures safely and effectively, with improved outcomes.
The Ongoing Evolution of Prostate Treatment
While robotic surgery has advanced rapidly, further innovations continue to enhance prostate care:
- New techniques like focal therapy target cancer cells precisely while preserving healthy tissue
- Research into refined surgical planning and simulation promises even better customization
- Future systems may enable remote telesurgery and further automation
Urologists now have an expanding arsenal of advanced options to battle prostate disease. Patients can expect continued progress in the coming years.
Final Thoughts on Selecting a Prostate Treatment Path
When facing prostate cancer or BPH, patients should educate themselves on all modern treatment alternatives before deciding on a path forward. Have an open discussion with your urologist regarding your lifestyle, priorities, and goals. Take advantage of cutting-edge technologies like robotic surgery when appropriate to achieve the best results.
Resources for Further Information and Support
Those confronting prostate issues can turn to reputable organizations like the American Urological Association and Us TOO International for up-to-date medical resources and community support. Patients should also read reviews and schedule consultations with top-rated urologists to find the right fit.