Most people are unfamiliar with ureter strictures and how they can impact urinary health.
By understanding what a ureter stricture is, what causes it, and how it's treated, you can better support loved ones facing this condition.
In this introductory article, we'll define ureter strictures, walk through their common symptoms and complications, and overview the anatomy involved in this condition.Learning the basics empowers you to compassionately discuss this diagnosis and its management.
Introduction to Ureter Strictures
A ureter stricture is an abnormal narrowing of the tube that carries urine from the kidney to the bladder. This narrowing, also called a ureteral stricture, often causes obstruction and backflow of urine.
Defining a Ureter Stricture
A ureter stricture refers to the narrowing of one or both ureters, which are the tubes that transport urine from the kidneys to the bladder. This narrowing is caused by scar tissue formation or external compression on the ureter. It can occur anywhere along the length of the ureter and leads to a partial or sometimes complete blockage of urine flow.
Some common causes of ureter strictures include:
- Kidney stones
- Past surgery or radiation therapy
- Injuries or trauma
- Congenital abnormalities
- Spread of cancers into the ureter
The medical term used to describe this condition is ureteral stricture.
Common Symptoms and Complications
A ureter stricture often causes the following symptoms:
- Pain in the side or back
- Frequent urinary tract infections
- Blood in the urine
- Kidney swelling (hydronephrosis)
- Kidney damage over time
If left untreated, a ureter stricture can lead to serious complications like kidney infections, stone formation, or even kidney failure in severe cases.
Basic Anatomy and Function
The ureters are muscular tubes about 10-12 inches long that carry urine from the kidneys to the bladder. A narrowing can occur anywhere along this pathway, often due to scar tissue formation or external compression. This frequently causes urine obstruction and backflow into the kidney, known as hydronephrosis.
Over time, a ureter stricture prevents proper drainage of urine from the kidney and causes progressive damage. Quick diagnosis and treatment are key to preserve kidney function and prevent infections.
What is the most common cause of ureteral strictures?
A common cause of ureteral strictures is ureteropelvic junction (UPJ) obstruction. This type of obstruction occurs where the ureter meets the renal pelvis in the kidney.
UPJ obstruction can be:
- Congenital: Present from birth due to abnormal development. This is the most common cause.
- From surgery: Scarring from surgical procedures can narrow the UPJ.
- From kidney stones: Stones passing through the UPJ can damage and scar the area.
- From inflammation: Swelling in the upper urinary tract can narrow the UPJ.
- From tumors: Cancerous or non-cancerous growths can compress the UPJ.
UPJ obstruction blocks urine flow from the kidney to the bladder. This backs up urine in the kidney, potentially causing damage. Prompt diagnosis and treatment is important to preserve kidney function.
Treatment options include surgery, stenting, or observation. Minimally invasive robotic surgery can be used to correct congenital UPJ obstructions. This allows quicker recovery than traditional open surgery.
What are the symptoms of a ureter stricture?
Ureter strictures can cause a variety of concerning symptoms that warrant medical evaluation. Some of the most common symptoms include:
- Flank pain - Due to urine backup and swelling, strictures may cause a dull, aching pain in the side and back. This tends to get worse over time.
- Abdominal pain - As the ureter and kidneys swell with backed up urine, pain may radiate to the upper abdomen as well. This pain may be intermittent or constant.
- Nausea and vomiting - Severe swelling and kidney dysfunction from an untreated stricture can lead to nausea and vomiting. This requires prompt treatment.
- Infection - Urine backup increases the risk of developing an infection in the kidney or ureter. This causes fevers, chills, fatigue and urgent urination.
- Fever - Fevers are a common sign of infection that has developed secondary to the stricture. This requires antibiotic treatment and drainage of the urine blockage.
In summary, a ureter stricture causes symptoms like pain, infection, nausea and fever due to severe urine backup and dysfunction. Anyone experiencing these concerning symptoms should promptly seek medical care for further evaluation and treatment. Catching a stricture early is key to preserving kidney function over the long term.
How is ureteral stricture treated?
Ureteral stricture can be treated through surgical or minimally invasive approaches, with the goal of permanently fixing the stricture and avoiding long-term stent use.
Some common treatment options include:
- Ureteral stent placement: A thin tube (stent) is inserted through the urethra and bladder to span the stricture, propping open the narrowed section of ureter. This relieves obstruction but is often temporary.
- Ureteral reconstruction surgery: Open surgery to remove the damaged section of ureter and reconnect healthy ends. This permanently fixes strictures but recovery can be difficult.
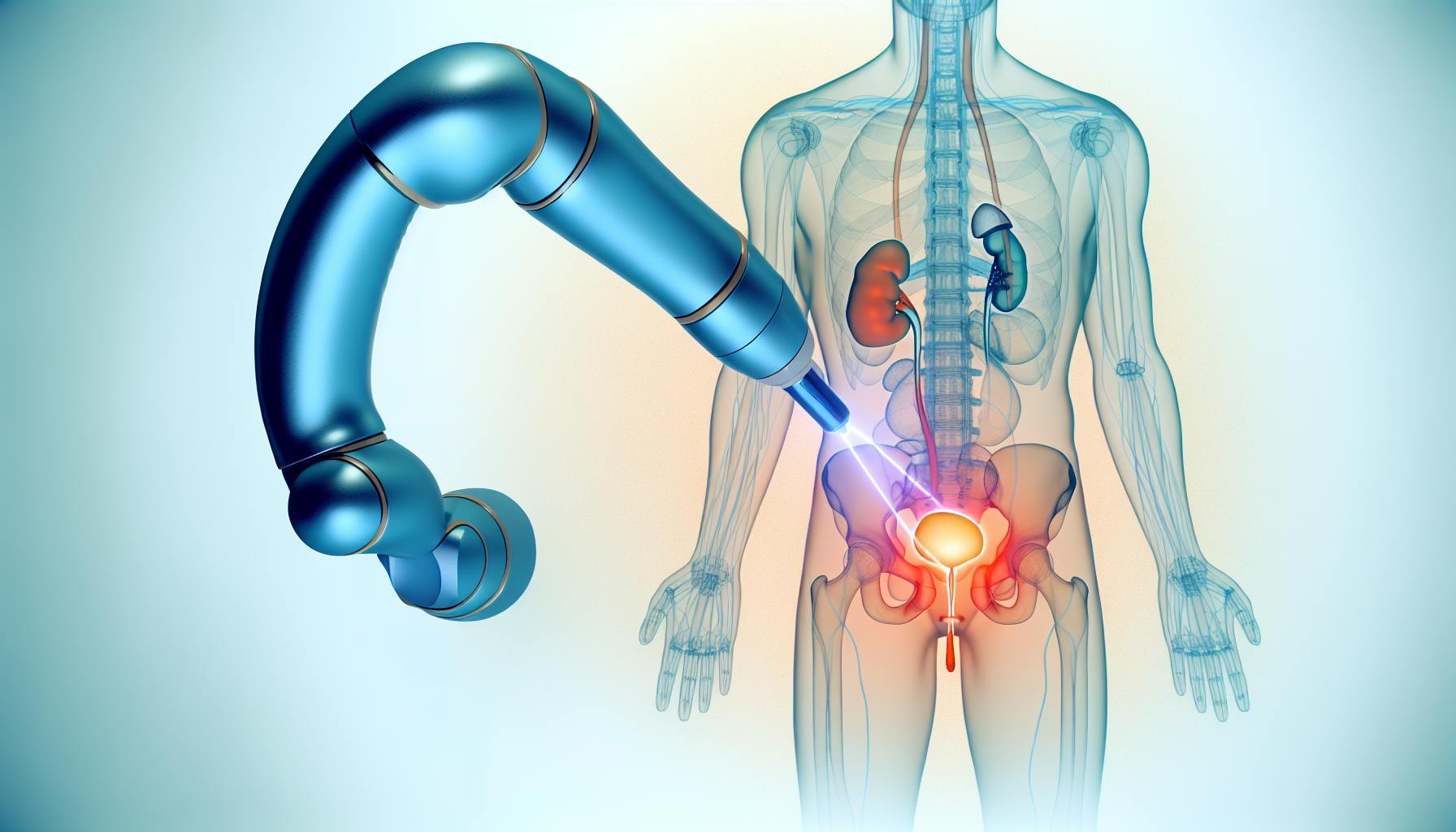
- Robotic ureteral reconstruction: A minimally invasive approach using robotic assistance. Smaller incisions lead to less pain, shorter hospital stays, and faster recovery than open surgery.
- Endopyelotomy: A stent with a balloon is inserted through a small abdominal incision to cut and expand the stricture using a laser or knife. This widens the ureter without completely removing the damaged section.
The best treatment option depends on multiple factors like stricture location, length, and cause. Your urologist will determine the optimal approach based on your unique clinical situation. The goal is to relieve obstruction and prevent kidney damage while minimizing invasiveness.
How serious is urethral stricture?
A urethral stricture is a narrowing of the urethra that can have serious consequences if left untreated. Over time, the stricture can worsen and cause permanent damage to the bladder and kidneys.
Some potential complications include:
- Recurrent urinary tract infections (UTIs)
- Blood in the urine
- Back up of urine into the kidneys, leading to hydronephrosis
- Permanent kidney damage and renal failure
The severity depends on the location and length of the stricture. The longer the stricture, the more serious the obstruction to urine flow. Strictures near the bladder tend to cause more issues than those further down the urethra.
That's why it's crucial to seek treatment for a urethral stricture as soon as symptoms appear. An untreated stricture tends to get worse over time and can eventually lead to life-threatening kidney problems.
The good news is that several effective treatments are available, especially if caught early. Options range from minimally invasive procedures to open surgery, depending on the case. With prompt diagnosis and management, most strictures can be successfully treated before irreversible damage occurs.
So in summary, a urethral stricture may start out mildly but can quickly become very serious if left unchecked. Pay attention to any urinary symptoms and see a urologist right away for evaluation and treatment. Catching it early is key to preventing complications down the road.
sbb-itb-89ec482
Understanding Ureter Stricture Causes
Ureter strictures, or abnormal narrowings of the tubes that carry urine from the kidneys to the bladder, can develop from a variety of causes. Understanding what leads to these strictures is key for diagnosis and determining the best treatment approach.
Iatrogenic and Surgical Causes
Past surgeries, radiation treatment, or improper catheter placement in the urinary tract area can create scar tissue that narrows the ureter over time. Common culprit procedures include:
- Hysterectomy
- Prostate cancer surgeries
- Kidney stone removal surgeries
- Radiation for pelvic cancers
- Long-term ureteral stent placement
When instruments or scopes are placed for these procedures, the delicate ureter lining can be damaged. As healing occurs, scar tissue forms and slowly contracts around the ureter, narrowing the pathway over months or years.
External Compression and Retroperitoneal Fibrosis
Structures near the ureter, such as cancers, blood vessels, or tissues, can sometimes compress the ureter from the outside and cause a stricture. Examples include:
- Retroperitoneal fibrosis - Fibrous tissue wraps around structures near the back of the abdomen, including the ureters. This constricts urine flow over time.
- Endometriosis - Uterine tissue grows outside the uterus and can surround/compress the ureter.
- Cancers - Tumors wrapping around the ureters narrow their diameter.
Congenital Ureteral Strictures
Some babies are born with congenital defects that obstruct urine drainage from the kidneys. These include:
- Ureteropelvic junction (UPJ) obstruction - The section where the ureter meets the kidney does not develop properly.
- Obstructing megaureter - An abnormally large, swollen ureter that twists shut.
Both can cause backpressure on urinary flow that damages the kidney. Scarring from this leads to a narrowing stricture later in life.
Inflammatory and Infectious Etiologies
Chronic inflammation or infection near the ureter can create scar tissue that slowly contracts around the ureter. Causes include:
- Repeated urinary tract infections (UTIs)
- Sexually transmitted diseases (STDs) like chlamydia and gonorrhea
- Tuberculosis
- Schistosomiasis
Identifying the underlying condition leading to a ureter stricture directs the proper long-term management approach to prevent recurrence.
Diagnosis of Ureter Strictures
Ureter strictures can often be challenging to diagnose. Doctors use a combination of approaches to fully evaluate the location, extent, and impact of any narrowings or blockages along the ureter tubes.
Medical History Review and Urinalysis
As a first step, the urologist will thoroughly review your medical history, including any past infections, surgeries, kidney stones, or other factors that could have led to scarring and strictures. Family history and a list of all medications and supplements are also reviewed.
A urinalysis is done to check for blood, protein, signs of infection or inflammation. Any concerning findings may warrant further testing.
Imaging Tests for Renal Obstruction
If obstruction is suspected, the doctor may order imaging tests to visualize the urinary system. Common options include:
-
CT scan: Provides detailed 3D cross-sectional images to view strictures and assess kidney function.
-
MRI: Uses magnets and radio waves to image soft tissues. Helps avoid radiation exposure from CT scans.
-
Ultrasound: Uses soundwaves to safely image the kidneys and ureters. Checks for hydronephrosis.
-
Retrograde pyelogram: Contrast dye is injected via a catheter placed through the urethra up to the ureters to highlight strictures.
Urodynamic Studies and Pressure Testing
Specialized tests can precisely measure urine flow rates and pressures within the urinary tract. These are used to confirm obstruction and check kidney function.
Examples include diuretic renography scans, Whitaker tests, and ureteral stenting trials. Stents with pressure sensors may also be placed.
Together, these approaches help pinpoint the location and severity of any ureter strictures present. This guides development of an optimal treatment plan.
Treatment Strategies for Ureter Strictures
Depending on the cause and location of the ureter stricture, various treatment options may be utilized.
Conservative Management and Monitoring
Mild cases of ureter strictures may only require periodic monitoring and medication if infection or pain is present. Doctors may prescribe antibiotics for infections or pain medications as needed. Imaging tests like ultrasounds or CT scans can track stricture severity over time. If the stricture does not worsen, conservative treatment may be sufficient.
Ureteral Stenting Procedures
For moderate ureter strictures causing recurring infections or kidney damage from obstruction, ureteral stents may be placed. A thin, hollow tube is inserted through the urethra and bladder before being positioned in the ureter, bypassing the stricture. This stent creates an open passageway for urine to flow from the kidney to the bladder normally. Stents are typically temporary but may be exchanged regularly if chronic stenting is required.
Surgical Reconstruction and Robotic-Assisted Surgery
In severe cases where a ureter is extremely narrowed or completely blocked, the damaged section can be surgically removed and the healthy ends reconnected. This delicate reconstructive procedure is often performed robotically or laparoscopically for greater precision. Smaller incisions lead to less pain and faster recovery compared to open surgery. Success rates for ureter reconstruction are usually high, especially for single strictures below 10 centimeters.
Urinary Diversions in Severe Cases
If the ureter stricture is too long or otherwise unable to be repaired, a urinary diversion may be necessary. This involves surgically redirecting urine flow externally through an opening (stoma) in the abdomen called a urostomy or ileal conduit. Urine may also be diverted internally to drain directly from the kidney to the bowel. While avoiding kidney damage, diversions require lifelong external catheter use or self-catheterization to empty urine.
Post-Treatment Recovery and Support
Proper aftercare and follow-up help ensure optimal healing and functioning of repaired ureters over the long term.
Post-Surgical Care and Recovery
After ureter stricture surgery, doctors provide detailed instructions for wound care, medication, activity restrictions, diet, and signs of complications to monitor. This helps ensure proper healing and prevents infection or other issues. Typical guidelines include:
- Keeping the incision clean and dry to prevent infection
- Taking prescribed antibiotics and pain medications as directed
- Avoiding strenuous activity or heavy lifting for 4-6 weeks
- Staying well hydrated by drinking adequate fluids
- Eating a balanced diet with sufficient protein and nutrients for healing
- Watching for signs of infection like fever, nausea, or increased pain/swelling
Following doctor's orders carefully during recovery is crucial for allowing repaired ureters to heal fully. Most patients need to take 4-6 weeks off work, avoiding strain on the area. With time and care, individuals can return to normal functioning.
Ongoing Follow-Up and Monitoring
After recovering initially, periodic follow-up visits assess progress. Doctors order urine tests, bloodwork, and imaging scans to check kidney function, urine flow, and monitor for recurring infection or strictures. If repaired areas narrow again, additional treatment may be needed.
Examples of follow-up testing include:
- Urinalysis: Checks for blood, bacteria, or other abnormalities
- Creatinine blood tests: Assess kidney filtration rate
- CT scans: Provide images of ureters to check repair status
- Ultrasounds: Use soundwaves to visualize urine flow
Based on testing, doctors determine if further stenting or surgery is necessary. Ongoing monitoring ensures long-term success of stricture repairs.
Lifestyle Adjustments for Renal Health
Making certain diet and lifestyle changes can also help repaired ureters function properly long-term:
- Stay hydrated by drinking 6-8 glasses of fluids daily
- Avoid bladder irritants like caffeine, alcohol, citrus juices
- Try pelvic floor therapy to improve muscle control
- Urinate regularly instead of delaying need to go
- Take warm baths to relieve discomfort
With some adjustments, individuals can support their body’s efforts to heal completely. Caring properly for post-surgical ureters promotes optimal recovery.
Navigating Urology Care for Ureter Strictures
Those experiencing potential symptoms of ureter strictures should promptly consult a urologist or nephrologist for specialized diagnosis and treatment.
Finding Specialized Urology Training and Expertise
When seeking care for a potential ureter stricture, it is important to find a urologist or nephrologist who has specialized training and expertise in this area. Board certification indicates that the physician has completed an accredited residency program and demonstrates a commitment to lifelong learning. Additionally, look for a doctor who has fellowship training, as this provides focused education on complex conditions beyond the initial residency. For instance, Dr. Canes has over 18 years of specialized experience in robotic surgery for urologic conditions. This level of expertise is vital when diagnosing and developing an appropriate treatment plan for ureter strictures.
Ideally, the urologist should also be affiliated with a major academic medical center, which signals access to the latest research and techniques. Large urology groups may also have multiple subspecialists to provide collaborative care. When researching physicians, look for consistently high patient satisfaction scores, awards and recognitions, an academic appointment, and a track record of positive surgical outcomes. This helps identify urologists with exceptional training to accurately assess ureter strictures.
The Value of Second Opinions in Urology
Given the complex nature of ureter strictures, it is often wise to seek multiple professional opinions when weighing treatment options. This provides reassurance that the diagnosis and plan are appropriate for your individual case. The collective expertise of different specialists can shed light on alternative therapies to consider. For instance, one physician may advise an open surgical procedure while another recommends an endoscopic or robotic minimally invasive surgery. Understanding all options allows patients to make the most informed decision.
Additionally, second opinions give peace of mind that the initial clinical impressions are accurate. They can clarify uncertainties, answer additional questions, and instill confidence moving forward. Patients have the right to explore different perspectives while finding the urologist they feel most comfortable with. Overall, gathering multiple viewpoints leads to greater patient empowerment and involvement in their own care.
The Role of Ongoing Urology Research in Patient Care
The field of urology continues to rapidly advance through dedicated research at academic institutions and medical conferences. Patients should look for urologists who actively participate in research and integrate findings into their clinical practice. For example, Dr. Canes holds a faculty appointment at Tufts University School of Medicine, allowing him to apply cutting-edge knowledge in patient care while also training future urologists.
Staying abreast of the latest studies provides insights into new diagnostic tools, expanded knowledge of disease processes, and innovative surgical techniques. Research may uncover improved methods of imaging strictures, enhanced stenting options to relieve obstruction, emerging robotic platforms, and novel postoperative protocols to prevent recurrence. Patients directly benefit from physicians who continually expand their expertise. Ultimately, an evidence-based approach drawing from ongoing research helps optimize and personalize treatment plans for those with ureter strictures.
Conclusion: Key Takeaways on Ureter Strictures
Ureter strictures can be a complex condition caused by a range of factors. If left untreated, they can lead to serious complications like kidney damage or failure. However, with prompt diagnosis and appropriate treatment, outcomes can be positive. Here are some key takeaways:
Recap of Ureter Stricture Fundamentals
- Ureter strictures are an abnormal narrowing of the tubes (ureters) that carry urine from the kidneys to the bladder
- Common causes include kidney stones, infections, radiation therapy, trauma, surgery, etc.
- Symptoms like flank pain, fever, nausea can indicate obstruction
- Tests like CT scans, MRIs, ultrasound, and ureteroscopy help diagnose
- Strictures need to be addressed quickly to prevent permanent kidney damage
Highlighting Treatment Modalities
- Treatment options range from stenting to open surgery
- Minimally invasive approaches like endoscopic surgery or robot-assisted surgery are often preferred
- In severe cases, partial kidney removal or kidney transplantation may be required
- Follow-up care with stenting changes is crucial to prevent recurrence
Emphasizing Recovery and Long-Term Support
- Close follow-up care allows assessment of treatment effectiveness
- Ongoing stenting with gradual increases between changes may prevent restenosis
- Lifestyle changes to prevent infection and manage related conditions are key
- Lifelong monitoring helps preserve kidney function and identify any new obstructions early
The key is early intervention and comprehensive long-term care. With the right treatment plan and support, positive outcomes are possible even for complex ureter strictures.