Undergoing surgery can be an intimidating experience. When facing a radical prostatectomy, patients likely agree that having a full understanding of the procedure is critical for peace of mind.
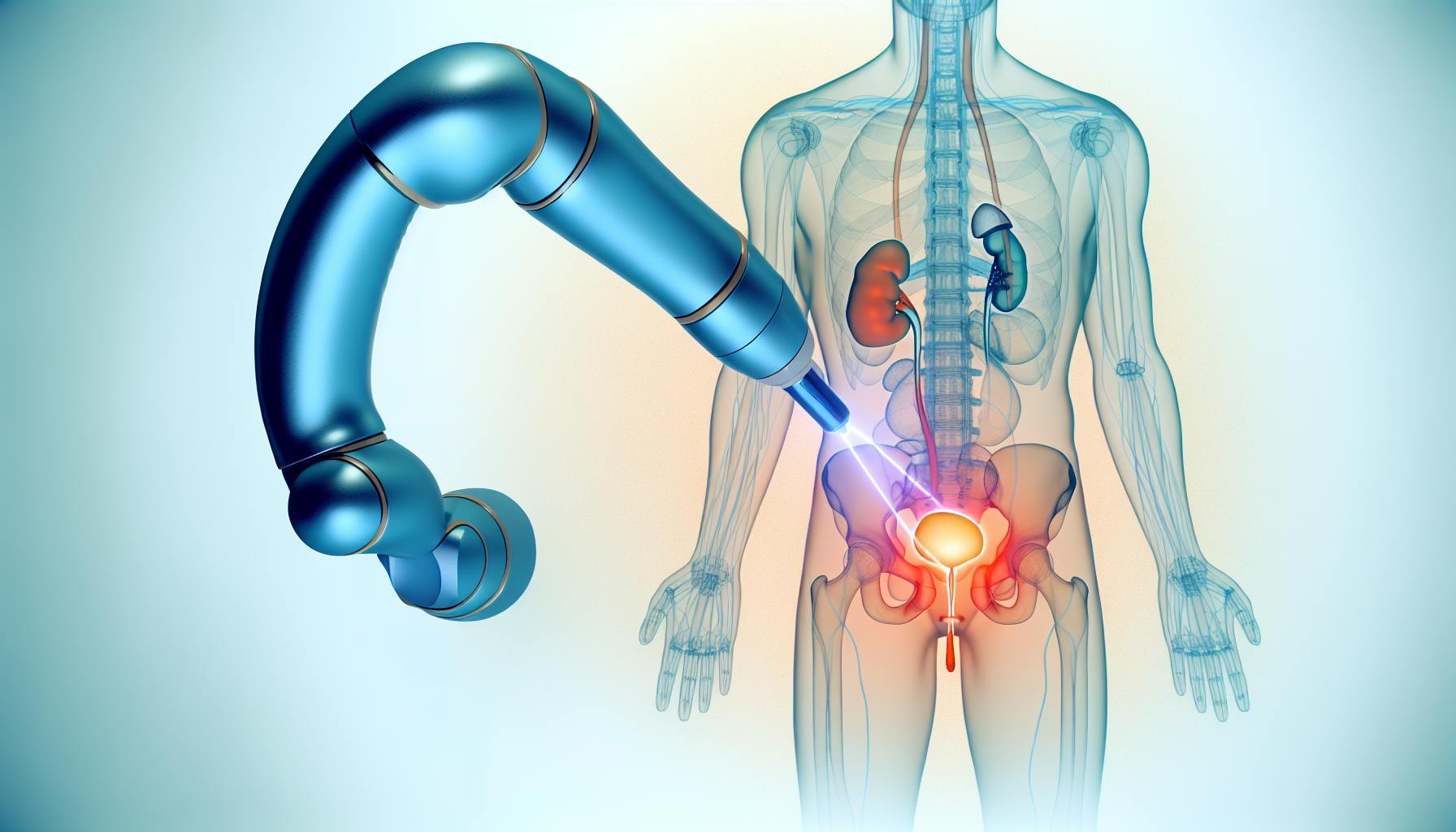
This guide on robot-assisted radical prostatectomy (RARP) surgery aims to educate patients on what to expect before, during, and after the operation.
We will overview the RARP technique, compare it to traditional prostate removal, outline the step-by-step surgical process, and detail recovery expectations and potential outcomes. With comprehensive information on the RARP journey, patients can feel informed, prepared, and reassured.
Introduction to Robot-Assisted Radical Prostatectomy (RARP)
This section provides an overview of RARP surgery, including its purpose in treating prostate cancer, the robotic surgery approach, and the benefits for patients.
Understanding RARP: A Modern Approach to Prostate Cancer
RARP is a minimally invasive form of pelvic surgery used to treat prostate cancer. It involves the surgical removal of the prostate gland along with some surrounding tissue. RARP utilizes a robotic interface that allows the surgeon to perform the procedure through tiny incisions using small instruments mounted on robotic arms. This enhances precision, flexibility, and control during the surgery.
The goal of RARP is to completely remove the cancerous prostate while preserving continence and sexual function. This is achieved through delicate nerve-sparing techniques enabled by the robotic platform. RARP provides several advantages over traditional open radical prostatectomy, including reduced blood loss, shorter hospital stays, faster healing, and lower risk of complications.
Overall, RARP is considered a highly effective option for removing prostatic cancer while minimizing side effects. The procedure allows precise cancer excision through a minimally invasive approach.
Anticipating the Success Rate of Robotic Prostatectomy
Studies show RARP has excellent outcomes for treating prostate cancer. Success rates are determined by several factors:
- Cancer stage - Earlier stage prostate cancer has higher RARP success rates. With localized cancer, studies report 10-year biochemical recurrence-free survival over 90%.
- Surgical margins - Negative surgical margins, meaning no cancer cells left behind on the excision site, are achieved in 80-90% of RARPs. Positive margins raise recurrence risk.
- Nerve-sparing - Preserving nerves for erectile function and continence during RARP boosts quality of life after surgery. High-volume surgeons perform optimal nerve-sparing.
- Surgeon experience - Success rates improve significantly based on a surgeon's RARP case volume and years in practice. Expertise matters.
While individual factors vary, patients can reasonably expect 80-95% 10-year biochemical recurrence-free survival from RARP in experienced hands. Continence and erectile function recovery is also favorable.
Comparing RARP with Traditional Radical Retropubic Prostatectomy
RARP differs from conventional radical retropubic prostatectomy (RRP) in several key ways:
- Smaller incisions - RARP uses 5-6 tiny abdominal incisions versus one large RRP incision. This reduces pain and scarring.
- Enhanced visualization - RARP provides a magnified 3D view of the prostate anatomy for improved surgical accuracy.
- Reduced blood loss - Average RARP blood loss is around 200 ml versus over 500 ml for RRP, resulting in fewer transfusions.
- Shorter hospitalization - Patients usually leave the hospital 1-2 days after RARP rather than 3-5 days with RRP.
- Quicker recovery - Healing from small RARP incisions is faster than a large RRP incision. Most patients return to normal activities in 2-3 weeks after RARP rather than 6-8 weeks after RRP.
In summary, RARP facilitates better outcomes through more precise, minimally invasive surgery enabled by robotic assistance. Patients undergoing RARP can expect a smoother procedure, shorter hospitalization, less pain, and faster recovery compared to traditional open radical prostatectomy.
What is RARP surgery?
Robotic assisted radical prostatectomy (RARP) is a minimally invasive surgical procedure to remove the prostate gland and surrounding tissue to eliminate prostate cancer. It is performed using a robotic surgical system that allows the surgeon to operate with enhanced vision, precision, and control.
Some key things to know about RARP surgery:
- It is one of the most common treatments for localized prostate cancer, along with open radical prostatectomy and radiation therapy. RARP accounts for 85-90% of radical prostatectomies performed.
- The goal of the surgery is to completely remove the prostate and seminal vesicles, while preserving continence and sexual function.
- It involves making 5-6 small incisions in the abdomen. The robotic arms and camera are inserted through these ports. This is less invasive than traditional open surgery.
- Patients are placed in a steep Trendelenburg position during surgery to allow the abdominal contents to shift away from the pelvis for better access.
- The surgeon sits at a console and controls the robotic arms to meticulously dissect the anatomy. This provides enhanced 3D visualization and dexterity compared to open surgery.
- After the prostate is removed, the bladder neck is connected to the urethra in a watertight fashion (anastomosis). This is a critical step.
- Patients usually stay 1-2 nights in the hospital. Typical recovery is 2-4 weeks.
In experienced hands, RARP can successfully eliminate prostate cancer while minimizing side effects like incontinence and impotence. Patients should select a surgeon based on experience, technique, and outcomes data.
Can you still have an erection if your prostate is removed?
Erectile dysfunction is a potential risk following radical prostatectomy surgery to remove the prostate gland due to prostate cancer. However, with advancements in nerve-sparing techniques, many men are still able to regain erectile function over time.
The nerves and blood vessels that control erections lie very close to the prostate gland. During surgery, the surgeon attempts to avoid damaging these delicate nerves and vessels to maximize the chances of preserving erectile function.
- With a nerve-sparing radical prostatectomy, studies show that 40-87% of men will regain erectile function sufficient for intercourse within 2 years after surgery. This continues to improve with more time.
- Recovery of erections can be a slow process, often taking 12-24 months. Factors like age, pre-surgery erectile function, and response to ED medications impact outcomes.
- Treatments like penile rehabilitation therapy, medications, injection therapy, vacuum devices and penile implants can aid those still struggling with ED after 2 years.
So while erectile dysfunction remains a risk, a nerve-sparing approach offers many men a good chance of recovering erections after radical prostatectomy. Discussing expectations and treatment options with your urologic oncology surgeon is important.
What is life expectancy after robotic prostatectomy?
Based on studies of patients who have undergone robotic prostatectomy (RARP) for localized prostate cancer, the average life expectancy exceeds 10 years post-surgery. However, many factors influence life expectancy, including:
- Age and overall health: Younger, healthier men at the time of surgery generally have better outcomes. Men over age 70 or with other health issues may have shorter life expectancies.
- Cancer stage and grade: If the cancer is caught early while still localized in the prostate, prognosis is usually excellent after surgery. However, if the cancer has spread to lymph nodes or beyond, life expectancy declines.
- Surgical approach: RARP utilizes tiny incisions for less blood loss, shorter hospital stays, and faster recovery. Open radical prostatectomy and laparoscopic procedures have fallen out of favor due to advantages of the robotic technique.
- Surgeon experience: Highly experienced surgeons like Dr. Canes perform hundreds of successful RARPs, improving outcomes. Less experienced surgeons may have higher rates of cancer recurrence and complications.
- Ongoing monitoring: Regular PSA tests, digital rectal exams, MRIs and potential radiation or hormone therapy help maximize longevity by catching any recurrence early.
In summary, choosing robotic prostatectomy performed by a surgeon like Dr. Canes offers patients the best chance at long-term survival and quality of life after prostate cancer treatment. Committing to follow-up monitoring and healthy lifestyle choices post-surgery also improves life expectancy.
How long does it take to recover from a robotic prostatectomy?
With robotic-assisted radical prostatectomy (RARP) surgery, the recovery time is typically 2-3 weeks. However, full recovery can take up to 6 weeks depending on the patient's age, health status, and procedure specifics.
Here is what patients can expect for recovering after RARP surgery:
- Hospital Stay: Patients usually go home the same day.
- First 2 Weeks: Early recovery focuses on managing pain and regaining mobility. Patients should take it very easy, get lots of rest, avoid lifting anything over 5-10 pounds, and walk for short periods each day. Urinary catheter is in place during this time, for the first 7 days.
- Weeks 3-4: Most patients have catheters and drainage tubes (if present) removed around 1 weeks post-op. They can start doing light activity but should still avoid strenuous exercise. Some urinary incontinence and erectile dysfunction are common initially but often improve with time and treatment.
- Week 5-6: If recovery remains on track, patients can ease back into their regular routines. Most people can return to desk jobs or light activities at this point but should still avoid heavy lifting and high impact exercise until cleared by their doctor.
So in summary, allow 2-3 weeks for an initial recovery with limited activity, but a full 6 weeks before resuming normal work and exercise routines after RARP surgery. The good news is most patients can expect a high cancer cure rate and preservation of urinary/sexual function over time with this state-of-the-art procedure.
Evaluating Candidacy for RARP Surgery
RARP, or robot-assisted radical prostatectomy, is a minimally invasive surgical procedure to remove the prostate gland as a treatment for prostate cancer. Determining if a patient is a good candidate for RARP surgery involves carefully assessing both the stage of their prostate cancer as well as their overall health and anatomy.
Assessing Prostate Cancer Stage for RARP Eligibility
The stage of a patient's prostate cancer, meaning how far it has progressed, is a key factor in evaluating their eligibility for RARP. Typically, RARP is most appropriate for patients with localized prostate cancer that has not spread beyond the prostate. Specifically, RARP tends to be recommended for:
- Stage I prostate cancer where the tumor is small and contained within the prostate
- Stage II prostate cancer confined within the prostate but more advanced than Stage I
- Some cases of Stage III prostate cancer where the cancer has spread just outside the prostate capsule
If the prostate cancer is more advanced and has metastasized more extensively, alternative treatments like radiation or hormone therapy may be more suitable than surgery.
Considering Patient Health and Anatomy for Robotic Surgery
Aside from cancer staging, a patient's overall health and anatomy are also important considerations for RARP candidacy. The robotic surgery does require the patient to be in a steep head-down position for an extended period, so issues like obesity or heart/lung conditions may preclude eligibility. Specific anatomical factors surgeons evaluate include:
- Presence of a large median lobe of the prostate which can complicate the surgery
- Prior abdominal or pelvic surgery like hernia repair that may impact surgical approach
- Size of the prostate gland itself
Carefully reviewing the patient's health and anatomy using imaging tests helps determine if RARP is appropriate or if open/non-robotic surgery may be safer.
Identifying Best Nerve-Sparing Prostate Surgeons
For optimal outcomes from RARP, it is advisable to select a surgeon specially trained in nerve-sparing techniques. This delicate surgery preserves the fine nerves and blood vessels involved in continence and sexual function surrounding the prostate. When performed by an experienced robotic surgeon, RARP can successfully remove prostate cancer while minimizing side effects.
Key factors to look for when choosing a prostate surgeon include:
- Fellowship training dedicated specifically to robotic prostatectomy
- High surgical volume including >100 RARP cases per year
- Consistently high patient satisfaction scores for urinary and erectile function after RARP surgery
Selecting the right surgeon can help ensure the best possibility of cure while retaining quality of life after prostate cancer treatment.
sbb-itb-89ec482
Preoperative Preparations for RARP
Completing the necessary preoperative preparations is an important step to ensure a safe and successful RARP surgery. This involves undergoing assessments to evaluate surgical readiness, adjusting medications and lifestyle to optimize health pre-surgery, and understanding procedures like Foley catheter placement.
Completing Necessary Preoperative Assessments
Before undergoing RARP surgery, patients will need to complete certain medical tests and evaluations, including:
- Physical Exam: Assesses overall health, heart and lung function, etc.
- Blood Tests: Checks blood cell counts, electrolytes, kidney and liver function.
- EKG/ECG: Records heart's electrical signals to uncover abnormalities.
- Chest X-Ray: Creates images of lungs and heart to spot issues.
- Anesthesia Evaluation: Reviews health history and determines anesthesia plan.
These assessments help uncover any underlying conditions that need addressing before surgery. They also provide a baseline to compare progress during recovery.
Adjusting Medications and Lifestyle Prior to Surgery
To reduce surgical risks, patients may need to make certain adjustments, such as:
- Stopping blood thinners: Helps avoid bleeding complications. May require substitutes.
- Starting stool softeners: Prevents constipation from pain meds.
- Quitting smoking: Lowers infection risk and supports healing.
- Healthy diet: Provides strength and speeds recovery.
- Light exercise: Improves fitness for surgery and recovery.
Making these changes 1-2 weeks before surgery, under a doctor's supervision, best prepares the body.
Understanding the Role of the Foley Catheter in RARP
During RARP, a Foley catheter is inserted into the urethra and bladder. This flexible tube has several key functions:
- Drain urine while the new bladder and urethra connections heal after prostate removal.
- Monitor urine output to ensure adequate kidney function.
- Identify bleeding or leaks early through urine color changes.
- Enable imaging tests to assess healing.
- Prevent narrowing or scarring of urethral connections.
The catheter is typically left in place for 1-2 weeks post-surgery before removal. While uncomfortable, it plays an important role in the RARP process.
Robotic Prostatectomy Procedure Steps
Initiating the Procedure: Anesthesia and Trendelenburg Position
The RARP procedure begins with the administration of general anesthesia to ensure the patient remains comfortable and pain-free throughout the surgery. Once anesthesia has taken effect, the patient is positioned in a steep head-down angle known as the Trendelenburg position. This allows the abdominal contents to shift away from the pelvis, giving the surgeon clear access to the prostate.
Performing Pelvic Lymphadenectomy and Lymph Node Dissection
After safely positioning the patient, the surgeon will make small incisions to insert laparoscopic instruments and a camera. This allows an inspection of the pelvic anatomy on-screen. The surgeon then removes lymph nodes around the prostate to test for cancer spread. This lymph node dissection provides critical staging information to guide treatment.
Executing Prostate Removal and Anastomosis
With a precise view of the prostate, the surgeon utilizes the robotic instruments to carefully dissect the gland away from surrounding structures. Preserving key nerves and muscles is vital to maintain continence and sexual function after healing. Once freed, the prostate is removed through a small incision. The surgeon then reconnects the bladder neck to the urethra (anastomosis), allowing normal urination once the catheter is removed.
Concluding the Surgery: Ensuring Precision and Safety
After thoroughly irrigating the surgical area and checking for bleeding, the surgeon removes instruments and closes incisions. The patient is taken off anesthesia and brought to the recovery room once stable. A catheter remains in place during initial healing to allow the anastomosis site to fully seal. The surgeon later checks the anastomosis integrity before catheter removal. Post-op care focuses on safely restoring urinary control and sexual function.
Postoperative Care: Hospital Recovery Expectations
Monitoring and Managing Pain Post-RARP
After RARP surgery, patients can expect some level of pain or discomfort as the body heals from this major procedure. The medical team will work to monitor pain levels closely and manage symptoms to keep patients as comfortable as possible.
Common pain management techniques include:
- Patient-controlled analgesia (PCA), allowing self-administration of pain medication
- Oral pain medications like acetaminophen or prescription opioids
- Local anesthetic blocks near incision sites or surgical drains
- Ice packs applied to the abdomen to reduce inflammation
Nurses will assess pain levels frequently using a numeric rating scale from 0-10. Reporting honest feedback ensures proper pain control. As pain improves, medications can be adjusted to avoid over-sedation.
Navigating In-Hospital Recovery and Rehabilitation
The hospital stay after RARP usually lasts 1-3 days on average. This allows close monitoring as the body begins recovering. Patients can expect:
- Frequent vital sign checks
- Working with physical and occupational therapists on gentle movement and walking
- Receiving adequate nutrition and hydration
- Having surgical drains, wound dressings, and catheter cared for by nurses
- Being assessed for return of bowel and bladder function
As strength returns, therapists will focus on core and pelvic floor exercises, walking longer distances, climbing stairs, etc. Clearing certain milestones allows for safe discharge.
Planning for Discharge and Home Care
Prior to hospital discharge, the care team provides instructions on proper home care to promote continued healing, including:
- Guidelines for showering and changing dressings
- Signs of infection or complications to monitor
- Catheter management and drainage bag routines
- Administering prescribed medications
- Follow-up appointment scheduling
Family members are encouraged to participate in discharge education. Being prepared eases the transition home where further recuperation and rehabilitation occur. Most feel ready to return to normal routines within 1-2 weeks.
Home Recovery Expectations After RARP
Managing recovery expectations and adhering to care instructions after undergoing RARP surgery is crucial for optimal healing. This section outlines key guidelines for patients once they return home after their hospital stay.
Managing Catheter Care and Monitoring for Urinary Incontinence
- Carefully follow instructions from your surgeon and nurses regarding catheter care, including how to empty the drainage bag and keep the area clean.
- Note any changes in urine color or odor, as this may indicate infection.
- Track urinary leakage episodes to monitor progress. Some leakage is common initially after catheter removal.
- Practice Kegel exercises to help strengthen pelvic muscles and improve continence.
- Use protective pads as needed while regaining control. Most patients see gradual improvement over 6-12 months.
Adhering to Activity Guidelines to Prevent Hernia Repair
- Avoid lifting over 10-15 lbs for 4-6 weeks, as this can put strain on internal incisions.
- Increase walking daily, but refrain from strenuous exercise for at least 1 month.
- Support the abdomen when coughing or sneezing to avoid pressure on healing tissues.
- Stay hydrated and avoid constipation from pain medications.
- Carefully monitor the incision site for any bulging, redness or pain - potential signs of hernia requiring repair.
Scheduling Follow-Up Visits and Continence Assessments
- Attend scheduled follow-up appointments for wound checks, catheter removal, and continence evaluation.
- Discuss any lingering side effects with your surgeon, such as erectile dysfunction or incontinence. Further treatment plans can optimize functional outcomes over time.
- Routine PSA tests will monitor for cancer recurrence. Discuss frequency based on individual risk profile.
- Physical therapy can also help rebuild pelvic floor strength if leakage persists beyond 6-12 months.
Closely following your surgeon's at-home instructions facilitates safe healing after prostate cancer surgery. Tracking progress and communicating concerns during follow-ups is key for optimal recovery.
Understanding Potential Outcomes of RARP Surgery
RARP (robot-assisted radical prostatectomy) surgery is an effective treatment option for prostate cancer, with excellent long-term outcomes when performed by a highly skilled surgeon. However, as with any major procedure, patients should understand there are potential side effects to consider.
Evaluating the Success Rate of Robotic Prostatectomy
Multiple studies have shown RARP has a high success rate in removing cancerous prostate tissue. Patients can expect:
- Cancer-free outcomes (no detectable PSA) in 80-90% of cases after 5 years when performed by an experienced, high-volume surgeon.
- Recurrence rates under 10% when surgeons use a meticulous nerve-sparing technique. This compares favorably to open radical prostatectomy.
- Continued refinements in surgical techniques leading to even better outcomes over time.
When choosing a surgeon, patients should review credentials, training, experience levels, and patient testimonials to evaluate surgical success rates.
Addressing Urinary Continence and Erectile Dysfunction
Two common issues after RARP are temporary urinary incontinence and erectile dysfunction:
- Urinary Continence - Around 95% of patients regain full urinary control within 1 year of surgery. Pelvic floor physical therapy can help strengthen muscles.
- Erectile Dysfunction - With a nerve-sparing technique, erection recovery rates approach 80% after 1 year. Oral medications or penile injections can also help in some cases.
Proactive patient communication with the surgical team is key for managing expectations and making a full recovery on both fronts.
Factors Influencing Long-Term RARP Outcomes
Several factors affect long-term outcomes:
- Surgeon Technique - A surgeon's experience and nerve-sparing precision significantly impact urinary/sexual function.
- Additional Treatments - Some patients may need adjuvant or salvage treatments like radiation or hormone therapy for full cancer control.
- Health and Age - General health, age, existing conditions, and commitment to recovery programs influence results.
By selecting an elite surgeon and proactively engaging in recovery, patients can optimize their RARP success and quality of life after prostate cancer.
Conclusion: Summarizing the RARP Surgery Journey
Reflecting on the RARP Experience
RARP surgery marks a pivotal point in a prostate cancer patient's journey. From diagnosis to surgery prep to recovery, RARP requires dedication and perseverance. However, with proper education and support, men can enter surgery feeling empowered and optimistic.
Reflecting on the RARP process reveals the importance of choosing a skilled, communicative surgical team. Selecting experienced, high-volume surgeons directly correlates with better outcomes. Robotic prostatectomy offers unmatched precision and improved recovery - when performed by the right hands.
While RARP does not guarantee a cure, it provides the best chance for cancer control with fewer side effects. With realistic expectations, adequate post-op care, and routine monitoring, most men can enjoy good long-term results. RARP surgery equips patients to reclaim fulfilling lives post-prostate cancer.
Reiterating the Importance of Selecting Skilled Surgeons
A patient's choice of surgeon profoundly impacts RARP success. Extensive robotic surgery experience directly translates to better operative technique, fewer complications, enhanced recovery, and reduced risk of recurrence.
Seeking out fellowship-trained robotic surgeons with proven track records of excellence ensures patients receive the highest quality of care. Surgeons should willingly provide their case volumes, patient testimonials, and clinical outcomes data.
Opting for high-volume RARP surgeons with thousands of cases under their belt offers men the best possibility of regaining urinary control and erectile function after surgery. An expert, meticulous nerve-sparing technique prevents unnecessary trauma during prostate removal.
Looking Ahead: Life After RARP Surgery
While RARP offers an effective treatment for prostate cancer, patients must continue managing their health post-operatively. Expect regular PSA tests, digital rectal exams, and potential imaging to monitor for recurrence. Adhering to follow-up care enables early detection and intervention if needed.
Additionally, pelvic floor rehabilitation can help men regain continence and sexual function. Other supportive measures include Kegel exercises, medications, penile rehabilitation programs, counseling, and lifestyle changes. With dedication and expert guidance, most men see gradual, continual improvement over time.
RARP surgery equips prostate cancer patients to reclaim rich, fulfilling lives. Although the journey presents challenges, selecting skilled surgeons and embracing proper follow-up care enables optimistic outcomes. Patients should feel empowered to educate themselves, ask questions, and seek personalized treatment.