When diagnosed with upper tract urothelial carcinoma, most patients face difficult decisions regarding potential treatment pathways and outcomes.
By reviewing the available options for upper tract urothelial carcinoma treatment, including surgery, chemotherapy, immunotherapy, and clinical trials, patients can work with their care team to map out an informed treatment plan aligned with their goals and priorities.
In this article, we will explore the key treatment modalities utilized for upper tract urothelial carcinoma patients, weighing the risks and benefits of each approach, latest research, and expert insights on optimizing patient-centered care.
Introduction to Upper Tract Urothelial Carcinoma Treatment Options
Upper tract urothelial carcinoma (UTUC) is a rare cancer affecting the lining of the upper urinary tract, including the renal pelvis and ureter. This article will provide an overview of current and emerging treatment options for UTUC, highlighting the importance of risk stratification and personalized treatment pathways.
Defining Upper Tract Urothelial Carcinoma and Its Treatment Landscape
UTUC accounts for only 5-10% of urothelial cancers, with an incidence of 1-2 cases per 100,000 in Western countries. It shares many similarities with bladder cancer. The main treatment options include surgery, chemotherapy, radiation therapy, immunotherapy, and clinical trials. The choice depends on the stage, grade, and location of the tumor. A personalized approach focused on the patient's unique risk factors is key.
Diagnosing Upper Tract Urothelial Cancer
Accurate diagnosis is critical for effective UTUC treatment. Recommended tests include urine cytology to check for cancer cells, ureteroscopy to directly visualize the tumor, and CT or MRI scans to assess invasion. Staging biopsies may also be performed. These tests determine the tumor grade, stage, and aggressiveness, guiding treatment decisions.
Staging and Risk Stratification in UTUC
Staging provides crucial information about the tumor size, lymph node spread, and metastasis used to assign a cancer stage. Risk stratification also evaluates grade, multifocality, and location. Low-risk UTUC is typically managed with kidney-sparing approaches whereas high-risk disease requires more aggressive interventions.
Prognostic Factors Influencing Treatment Decisions
Lymphovascular invasion, high tumor grade, sessile architecture, and tumor necrosis predict poor outcomes in UTUC. Evaluating these pathological factors helps determine optimal individualized treatment to balance efficacy and quality of life.
Overview of Treatment Pathways for Upper Tract Urothelial Carcinoma
Standard interventions include surgery (nephroureterectomy or kidney-sparing procedures), chemotherapy, radiation therapy, immunotherapy, and clinical trials. Treatment decisions depend on risk stratification based on grade, stage, location, etc. Continued surveillance is crucial for detecting recurrence.
How do you treat upper urinary tract urothelial carcinoma?
Upper tract urothelial carcinoma (UTUC) treatment depends on the stage and grade of the tumor. The standard treatment for high-risk UTUC is radical nephroureterectomy, which involves surgical removal of the entire kidney, ureter, and bladder cuff. This is typically done regardless of the tumor location in the upper urinary tract.
There are several surgical approaches for radical nephroureterectomy:
- Open surgery - A large abdominal incision to access the kidney and ureter. This allows direct visualization of structures.
- Laparoscopic - Minimally invasive approach using small incisions and specialized tools. Provides good visualization while minimizing pain and recovery time.
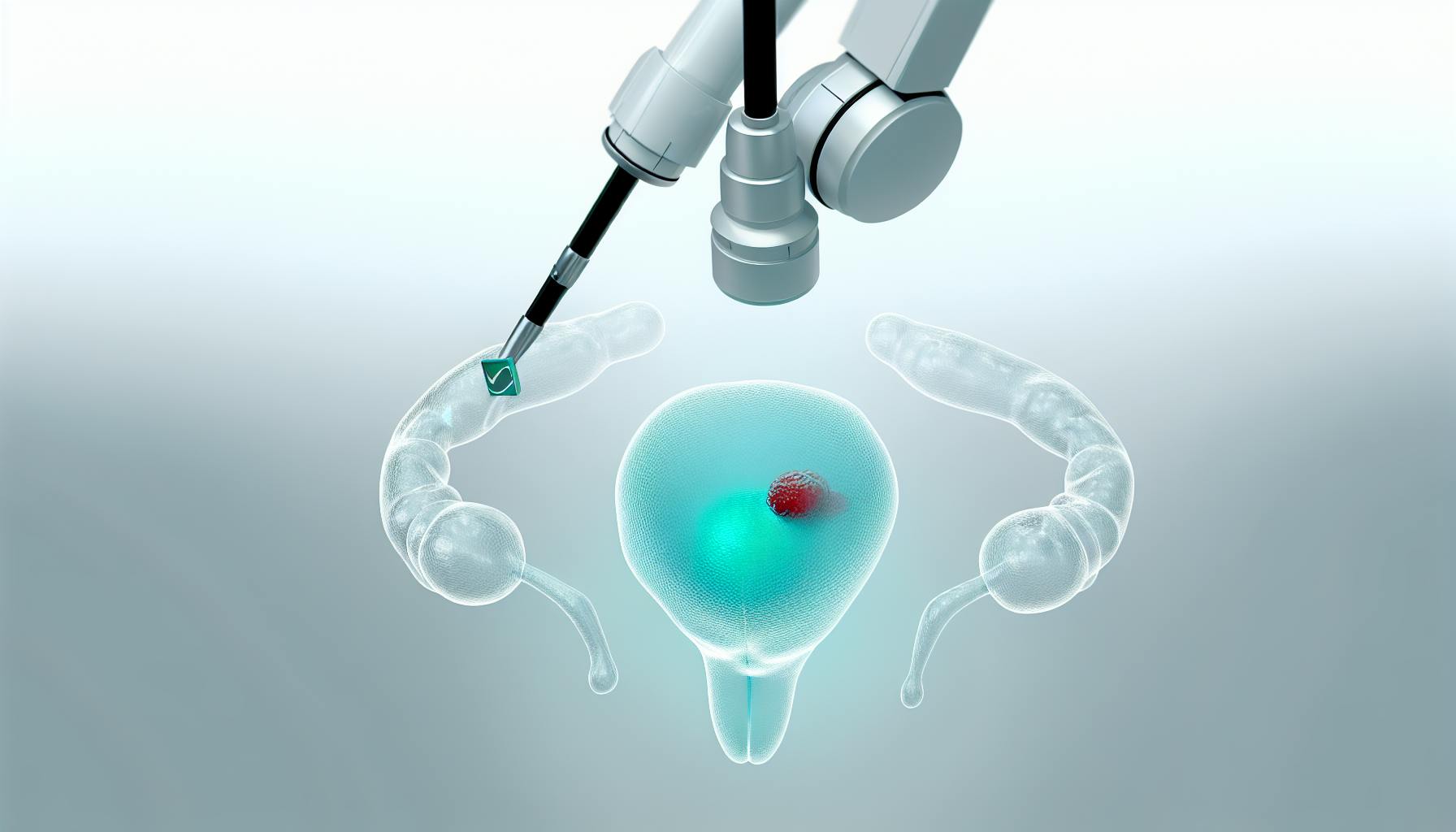
- Robotic surgery - Similar to laparoscopic but uses a robotic system controlled by the surgeon. Enables great precision and control.
Research shows that all these surgical approaches have similar oncological outcomes for organ-confined UTUC. The key factor is the complete removal of the bladder cuff, as failure to do so increases the risk of bladder cancer recurrence.
For low-grade, low-stage UTUC confined to the ureter or renal pelvis, kidney-sparing management may be an option instead of radical surgery. This can involve:
- Segmental ureterectomy
- Laser ablation
- Topical immunotherapy
Adjuvant chemotherapy is sometimes used after surgery to reduce recurrence risk. Emerging immunotherapies and precision medicine approaches are also being studied in clinical trials.
So in summary, radical nephroureterectomy is standard for high-risk disease, while kidney-sparing options may be suitable for some low-risk cases. All treatment decisions are based on careful risk stratification and assessment of each unique clinical scenario.
What is the survival rate for upper tract urothelial cancer?
Upper tract urothelial carcinoma (UTUC) is an aggressive disease with variable survival rates depending on the stage at diagnosis.
- For non-muscle invasive UTUC, the 5-year cancer-specific survival (CSS) rate is approximately 86%. These tumors are typically low grade and have not invaded beyond the inner mucosal layer.
- For muscle-invasive organ-confined UTUC, the 5-year CSS rate is around 70%. These tumors extend into the muscle wall but have not spread beyond the kidney or ureter.
- For locally advanced UTUC with extension into perinephric fat or adjacent organs, the 5-year CSS rate drops to 44%. Regional lymph node metastases are often present.
Prognosis worsens with more advanced stage, higher grade, lymphovascular invasion, and lymph node involvement. Close surveillance and consideration of adjuvant chemotherapy is warranted, especially for high-risk cases. Clinical trials evaluating novel systemic therapies and genomic profiling may provide new treatment options.
Overall, early detection and prompt surgical removal offers the best chance for long-term UTUC survival. Patient education on symptoms and routine screening for those at increased risk are critical for early diagnosis and optimal outcomes.
What is the surgery for upper tract urothelial carcinoma?
The most common surgery for upper tract urothelial carcinoma (UTUC) is radical nephroureterectomy. This involves removing the entire kidney, ureter, and surrounding fat in one piece. The goals of surgery are to remove all cancerous tissue and prevent recurrence.
Some key points about radical nephroureterectomy:
- Performed both open and robotically
- Removes kidney, ureter, adrenal gland, and Gerota's fascia
- Lymph nodes near the kidney may also be removed
- Kidney-sparing surgery may be an option for some patients
Additional considerations with surgery:
- Neoadjuvant chemotherapy before surgery may improve outcomes
- Adjuvant chemotherapy after surgery may eliminate residual cancer cells
Surgery remains the gold standard treatment for non-metastatic UTUC. An experienced urologic oncologist can determine if surgery is appropriate and which type of procedure is best suited for an individual’s unique situation. Regular follow up visits are necessary after surgery to monitor for potential recurrence.
sbb-itb-89ec482
What is the best treatment for urothelial carcinoma?
The best treatment approach for upper tract urothelial carcinoma depends on several factors, including the stage and grade of the cancer, patient health status, and treatment goals. Some of the main treatment options include:
Surgery
- Radical nephroureterectomy: Complete removal of the kidney, ureter, and surrounding tissue. This is often the first-line treatment for upper tract urothelial carcinoma.
- Kidney-sparing surgery: For some patients, only the tumor and part of the ureter may be removed to preserve kidney function.
Chemotherapy
- Neoadjuvant chemotherapy: Given before surgery to shrink the tumor and lower the risk of recurrence. Commonly used regimens include gemcitabine/cisplatin and methotrexate/vinblastine/doxorubicin/cisplatin (MVAC).
- Adjuvant chemotherapy: Given after surgery when there is a higher risk of recurrence. The same regimens may be used.
Immunotherapy and Clinical Trials
- Emerging immunotherapies like checkpoint inhibitors have shown promise in treating advanced urothelial carcinoma. Enrollment in clinical trials may provide access to these latest treatment options.
The best approach depends on each patient's unique situation. Dr. Canes will take all factors into account when determining the optimal upper tract urothelial carcinoma treatment plan for every patient.
Surgical Treatment Pathways for Upper Tract Urothelial Carcinoma
Surgery represents a cornerstone of UTUC treatment. We’ll explore the primary surgical options, including radical nephroureterectomy and kidney-sparing management, and their roles in treatment pathways.
Radical Nephroureterectomy for High-Risk UTUC
Radical nephroureterectomy involving complete kidney and ureter removal is often recommended for high-risk UTUC. This procedure involves surgically removing the entire kidney, ureter, and bladder cuff. It is considered the gold standard treatment for high-risk, muscle-invasive, or high-grade UTUC.
Radical nephroureterectomy provides excellent cancer control for high-risk disease. 5-year disease-specific survival rates range from 60-90% depending on pathologic stage. Complications include chronic kidney disease risk if the contralateral kidney function is impaired. Patients may require dialysis or kidney transplantation.
The Role of Lymph Node Dissection in UTUC Surgery
Lymph node dissection is recommended for patients with suspected lymph node metastasis. For non-metastatic UTUC, lymph node dissection has not shown clear survival benefit but may provide prognostic information to guide adjuvant chemotherapy.
The chances of occult lymph node metastasis depends on grade, stage, lymphovascular invasion, tumor architecture, and location. Template-based lymph node dissection increases staging accuracy. For suspected nodal disease, lymph node dissection is recommended.
Kidney-Sparing Management for Low-Risk UTUC
For select patients with low-risk UTUC, kidney-sparing approaches may be preferable to radical nephroureterectomy. This includes patients with significant comorbidities, solitary kidneys, or bilateral disease.
Kidney-sparing options include segmental ureterectomy or endoscopic ablation. These are options for patients with unifocal tumors <2cm, low-grade pathology, no invasion into muscle wall, and a normally functioning contralateral kidney.
5-year cancer specific survival rates of over 90% have been achieved with kidney-sparing management for appropriately selected low-risk patients. It preserves renal function while maintaining oncologic efficacy.
Postoperative Surveillance Following UTUC Surgery
Lifelong surveillance is imperative after UTUC treatment given the high rates of recurrence and risk of new tumors. Follow-up includes cystoscopy, urinary cytology, and CT urography at regular intervals. With recurrence, options include chemotherapy, radiation, or repeat surgery.
Upper tract imaging and ureteroscopy are also critical for detection of new upper tract tumors. More than 50% of recurrences manifest in the bladder. Thus, vigilant monitoring improves early identification and outcomes.
Recovery and Survivorship Post-UTUC Surgery
Following UTUC surgery, good self-care and long-term surveillance are vital. Excellent cancer control and survival rates over 5 years are achievable with appropriate patient selection and treatment.
Patients should focus on healthy habits and maintaining follow-up care. Support groups and counseling services can also help patients adjust after treatment. With proper recovery and monitoring, UTUC patients can enjoy long-term survivorship.
Chemotherapy in the Treatment of Upper Tract Urothelial Carcinoma
Chemotherapy plays an integral role in the management of upper tract urothelial carcinoma (UTUC). Both neoadjuvant chemotherapy prior to surgery and adjuvant chemotherapy after surgery have demonstrated benefits for select patients. Understanding how to optimize chemotherapy regimens and manage side effects is critical to effective UTUC treatment. Emerging immunotherapies also show promise to enhance outcomes when combined with chemotherapy.
Neoadjuvant Chemotherapy: A Pre-Surgical Strategy
Administering chemotherapy before surgery (neoadjuvant chemotherapy) has been associated with improved survival in patients with locally advanced UTUC. Multiple studies have shown that delivering 2-4 cycles of chemotherapy prior to nephroureterectomy can downstage tumors and eradicate micrometastases. Platinum-based regimens like gemcitabine + cisplatin or methotrexate, vinblastine, doxorubicin + cisplatin (MVAC) are commonly used. Patient selection is key - those with T2 or higher non-metastatic UTUC seem to derive the greatest benefit.
Adjuvant Chemotherapy: Post-Surgical Treatment
While less extensively studied than neoadjuvant chemotherapy, adjuvant chemotherapy after surgery may improve outcomes for high-risk UTUC patients. Particularly in cases of locally advanced disease or positive lymph nodes, adjuvant chemotherapy is often utilized to eliminate residual cancer cells. The same platinum-based regimens are typically given for 2-4 cycles post-operatively. Ongoing trials continue to refine criteria for adjuvant chemotherapy in UTUC.
Tailoring Chemotherapy Regimens for UTUC
Chemotherapy selection and dosing for UTUC should be personalized based on patient risk factors and tolerance. Those with renal dysfunction may require dose reductions or non-platinum regimens like gemcitabine or taxanes. Carboplatin can substitute for cisplatin in some cases. Younger, healthy patients may be candidates for dose-dense MVAC. Continued surveillance during and after chemotherapy is critical to assess efficacy and manage adverse events.
Managing Side Effects of Chemotherapy in UTUC Patients
Chemotherapy side effects like nausea, fatigue, neuropathy must be proactively addressed to maintain quality of life and treatment compliance. Anti-emetics, growth factors, pain medications can help mitigate symptoms. Clear patient education regarding side effects and prompt reporting of issues is essential. Sometimes treatment delays or reductions are warranted based on toxicity. Supportive care during chemotherapy is key for optimal UTUC management.
Emerging Chemotherapy and Immunotherapy Combinations
Exciting trials are underway combining immune checkpoint inhibitors with chemotherapy for UTUC. Agents like pembrolizumab and atezolizumab are being added to traditional platinum-based chemotherapy. Early results demonstrate improved response rates and survival compared to chemotherapy alone, with acceptable toxicity profiles. Biomarker analyses aim to determine which UTUC patients benefit most from chemoimmunotherapy. Further research is needed to optimize these combination regimens.
Advancements in Systemic Therapies for Upper Tract Urothelial Carcinoma
Emerging systemic therapies, including immunotherapy and targeted treatments, are expanding the arsenal against advanced UTUC. We'll explore the latest developments and their clinical implications.
Immunotherapy: A Breakthrough in UTUC Treatment
Immunotherapy with PD-1/PD-L1 inhibitors has led to a major shift in the treatment of advanced and metastatic UTUC. Multiple clinical trials have shown significant improvements in response rates and overall survival when these agents are used as monotherapy or in combination regimens.
Key points regarding immunotherapy for UTUC:
- PD-1/PD-L1 inhibitors like pembrolizumab, nivolumab, durvalumab, and avelumab have demonstrated antitumor activity and survival benefits in UTUC
- These agents now have FDA approvals for locally advanced or metastatic UTUC after platinum-based chemotherapy
- Ongoing trials are evaluating immunotherapy earlier in treatment algorithms, including in the neoadjuvant and adjuvant settings
- Combining immunotherapy with chemotherapy or other novel agents is an intense area of investigation to further improve outcomes
By enhancing the body's own immune response against UTUC, immunotherapy represents the most promising systemic therapy advance in decades. Continued research in optimal combinations and sequencing will expand use cases for these revolutionary treatments.
Antibody-Drug Conjugates: A Novel Approach
Antibody-drug conjugates (ADCs) have emerged as an innovative therapeutic strategy in UTUC. These agents combine a monoclonal antibody directed at antigens on tumor cells with a cytotoxic drug connected by a linker.
Key aspects of ADCs for UTUC:
- Enfortumab vedotin targets Nectin-4, which is highly expressed on UTUC cells
- In a pivotal trial, enfortumab vedotin produced a 44% response rate with 7.6 month median duration of response in metastatic UTUC
- Additional ADCs like sacituzumab govitecan and patritumab deruxtecan are under clinical investigation
- ADCs allow targeted delivery of chemotherapy to tumor cells while reducing systemic exposure
- Further research is needed to determine optimal use of these agents in UTUC protocols
ADCs permit a more personalized, precision-based approach to systemic therapy for advanced UTUC. As research continues, they may play a greater role earlier in the disease course.
Evaluating Targeted Therapies in Clinical Trials
Beyond immunotherapy and ADCs, small molecule inhibitors and other emerging systemic therapies are being assessed in UTUC through clinical trials.
Examples include:
- FGFR inhibitors: Targets fibroblast growth factor receptors implicated in UTUC progression
- PI3K/AKT/mTOR pathway inhibitors: Interfere with signaling pathways involved in cell proliferation and survival
- HER2 inhibitors: Block the HER2 receptor observed to be overexpressed in some UTUC cases
- Angiogenesis inhibitors: Prevent the formation of new blood vessels to cut off tumor growth
Determining the efficacy and safety of these treatments will shape future standards of care for advanced or high-risk UTUC. Molecular profiling of individual tumors can identify actionable targets for tailored therapy approaches.
Stratifying Patients for Combination Therapies
Rather than monotherapy, combination regimens leveraging immunotherapy, chemotherapy, and novel agents are likely to produce superior outcomes in UTUC. Key considerations for combination therapy include:
- Carefully selecting patients based on performance status, comorbidities, and treatment goals
- Monitoring for increased toxicity and side effects
- Identifying predictive biomarkers to guide personalized combinations
- Sequencing therapies for maximum duration of response
Clinical trials stratifying patients by risk factors and genomic features will provide data to refine combination therapy algorithms. This represents the leading edge in advancing toward more effective systemic treatments for UTUC.
Participating in Clinical Trials for Emerging UTUC Therapies
The pace of progress in UTUC therapies means clinical trials are indispensable for gaining access to the latest developments. Patients interested in emerging treatments should proactively engage with their care team about relevant studies.
Participating in clinical research enables patients to help define new standards of care while potentially benefiting from cutting-edge interventions. Supporting accrual of study participants is also key for advancing the evidence base in this rare disease. Patients should discuss options for enrollment at high-volume academic centers conducting novel UTUC trials.
Together with patients, researchers and clinicians will continue pushing toward the goal of making UTUC a chronically manageable condition with improved longevity and quality of life.
Concluding Insights on Upper Tract Urothelial Carcinoma Treatment
Upper tract urothelial carcinoma (UTUC) is an aggressive disease that requires prompt and effective treatment. As research continues to advance our understanding of UTUC biology and treatment responses, the future looks bright for improving patient outcomes.
Summarizing the Main Treatment Pathways for UTUC
The primary treatment options for UTUC include:
- Surgery - Radical nephroureterectomy with bladder cuff excision is the gold standard treatment for UTUC. Lymph node dissection and kidney-sparing management may be considered for select patients.
- Chemotherapy - Neoadjuvant chemotherapy prior to surgery as well as adjuvant chemotherapy after surgery have demonstrated survival benefits in high-risk UTUC cases. Platinum-based regimens are commonly used.
- Emerging Therapies - Immunotherapies, targeted therapies, and other novel agents are currently being evaluated in clinical trials for UTUC. These may expand treatment options in the future.
Anticipating Future Directions in UTUC Research
Ongoing research is investigating prognostic and predictive biomarkers to guide risk-stratified, personalized UTUC treatment plans. Additional studies are also evaluating emerging therapies like immunotherapy and targeted therapies. As research continues, we may be able to better select optimal treatments for each UTUC patient.
The Critical Role of Clinical Trials in Advancing UTUC Treatment
By rigorously testing new UTUC treatments, clinical trials establish improved standards of care over time. Patient participation is essential for progress. Those interested can ask their doctor about open trials.
Envisioning a Future of Improved Outcomes for UTUC Patients
Our increased understanding of UTUC biology and treatment responses raises hope for continued advances. Through ongoing research and clinical trials, we may continue to make great strides improving UTUC outcomes.
Final Thoughts on Upper Tract Urothelial Carcinoma Treatment
In conclusion, surgery and chemotherapy remain the standard treatments for UTUC today, but emerging options are on the horizon. Continued research and clinical trial participation will be key to further improving patient survival and quality of life. Patients diagnosed with UTUC should discuss all available treatment options with their doctor.